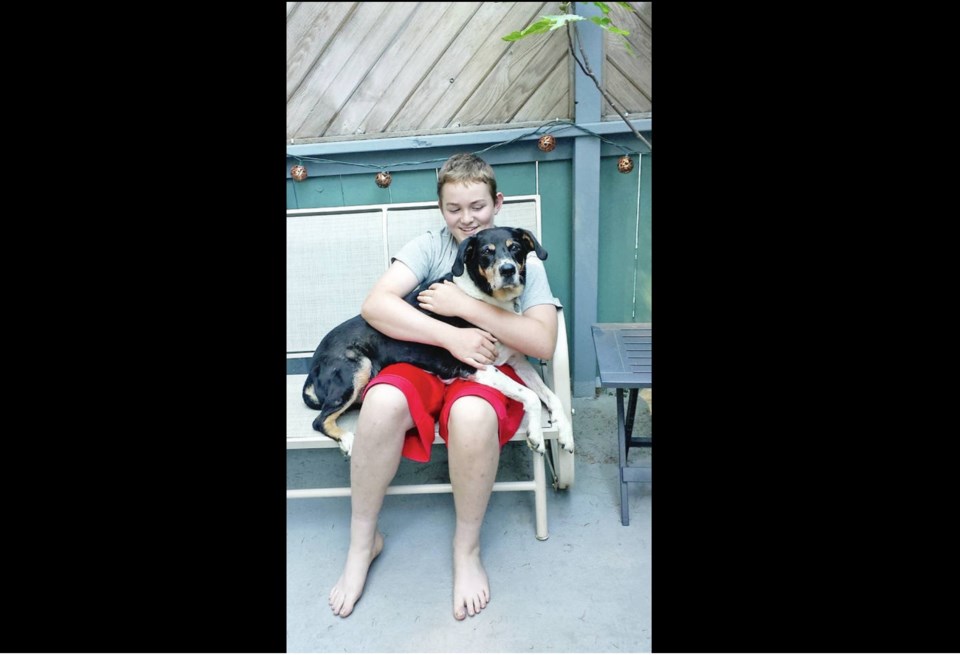
When Glenn and Denise Courtemanche stand in front of the wooden plaque in Goldstream Provincial Park in memory of their son Andre, who died by suicide in the park a few weeks ago, they remember a caring 16-year-old who adored his dog Max and loved to give family members hand-made gifts.
They also remember all the ways B.C.’s mental-health system failed their son.
In early December, when they discovered Andre had stopped taking his medication for depression and anxiety, the Courtemanches had called the youth crisis line and their family doctor. The doctor had referred Andre to a psychiatrist six months earlier, when the teen said his medication wasn’t working. But by late December, as Andre’s mental health deteriorated, the family still hadn’t received a call from a psychiatrist.
Denise pressed the family doctor to check on the referral. On Jan. 3, two days after Andre was last seen leaving his Cressida Crescent home and walking along the E & N rail line that abuts the backyard, the couple got a call about a psychiatric appointment in February.“I was angry,” Glenn Courtemanche said of the call that came too late.
“I was in disbelief,” Denise Courtemanche said. “I just told them: ‘You do realize this is the boy that’s missing?’”
Andre’s body was found Jan. 9 in Goldstream Provincial Park.
“There needs to be a more timely and immediate response when someone has the courage to come forward and ask for help,” said Denise Courtemanche.
Andre had been attending weekly support meetings at the Victoria Youth Empowerment Society since the spring of 2019, when he had a three-week stay in hospital to address a deep depression that left him suicidal. The teen had been struggling since the age of 14, when he was bullied as he started Grade 9 at Belmont Secondary School.
Andre’s mental health improved when he started attending the West Coast Centre for Learning, where he made some friends. He also started working out and lost 60 pounds, which his parents said boosted his confidence.
But his mother said the pandemic, which robbed Andre of his ability to see his grandparents in Port Alberni and isolated him from his friends, took a major toll on Andre’s health. He was also devastated by the August death of the family’s 15-year-old rescue dog, Max.
According to the Ministry of Mental Health and Addictions, children and youth trying to get their first visit with clinical or psychiatric mental-health services faced an average wait time of 54.5 days in 2019-20 — down from a 69.3-day average wait time three years before.
There are many ways for youth to access a psychiatrist, the ministry said, but the main one in Island Health is through Child and Youth Mental Health services under the Ministry of Children and Family Development, the process the Courtemanche family went through.
“After decades where mental health care was neglected, we know that many young people and their families still face long wait times for care and struggle to get help early,” Minister of Mental Health and Addiction Sheila Malcolmson said in a statement. She said the province is building a system of care “from the ground up” that focuses on early intervention and prevention.
Since Andre’s death, the family has heard from dozens of people who have lost a loved one to suicide, some in the same location at the Goldstream railway bridge, and those who have had their own struggles accessing mental-health supports.
“I hope that by us sharing our story, it lets other people know that they’re not alone and to seek the help that they deserve,” Denise Courtemanche said.
The couple, who held a memorial for Andre with a small group of immediate family on Jan. 21, said the community support has been incredible and they want to thank the first responders and everyone who helped search for Andre.
They hope some of the funds raised through an online fundraising page for barriers on the Goldstream bridge will go toward an outdoor program focused on youth mental health. They also want to organize a mental-health awareness walk that could happen every year on May 8, Andre’s birthday.
Island Corridor Foundation CEO Larry Stevenson said the group, which owns the bridge, is seeking expert advice on measures that could reduce the risk of suicides from the bridge. The foundation said it will provide an update on proposed solutions within days.
Jonny Morris, CEO of the Canadian Mental Health Association’s B.C. division, said barriers on the bridge is just one part of a complex set of measures that can prevent suicide deaths in B.C., the second leading cause of death for young people after motor vehicle crashes.
Morris said he understands that the B.C. government is trying to rebuild mental health and addiction resources after decades of underfunding. But he’s heard from many families like Andre’s who are frustrated with wait lists for mental health resources and feel like their children are falling through the cracks.
“When they’re waiting for care for a long time — and wait lists are a big part of the mental-health system — people change, their symptoms get worse and their trust in the system changes. The aim is to get to people help as early as possible,” Morris said. “There is absolutely an opportunity for this province’s health care system to become more responsive to the care of people who are suicidal.”
Anyone in mental-health crisis or who is having suicidal thoughts can call the Vancouver Island Crisis Line: 1‑888‑494‑3888.
The Ministry of Mental Health and Addiction said young people in Greater Victoria can obtain mental health supports at Foundry Victoria — which offers mental health care, substance use services, primary and sexual health care, youth and family peer support and social services — or through the Foundry Virtual online service at foundrybc.ca/virtual. The province said three new urgent and primary care centres, James Bay Urgent Primary Care Centre, North Q uadra Urgent Primary Care Centre and Westshore Urgent Primary Care Centre, also have clinicians who can provide same-day access.